Welcome to the Biotech Spotlight, a series featuring companies that are creating breakthrough technologies and products. Today, we’re looking at Gracell Biotechnologies, which is developing both autologous and allogeneic CAR-T cell therapies for solid tumors.
In focus with: William Wei Cao, CEO, chair and founder, Gracell Biotechnologies
Gracell Biotechnologies’ vision: With more than 30 years of experience in cell therapy R&D, including founding two startups and establishing more than 100 patents and applications for advanced cell therapies, Wei Cao is positioning his latest venture, Gracell Biotechnologies, to solve the biggest issues involved with CAR-T cell therapies: manufacturing time, cell quality, cost and use as a first-line therapy for solid tumors. Founded in 2017, the global clinical-stage biopharma company is pursuing the unusual path of developing both autologous and allogeneic products through its FasTCAR and TruUCAR technology platforms and Smart CART technology module.

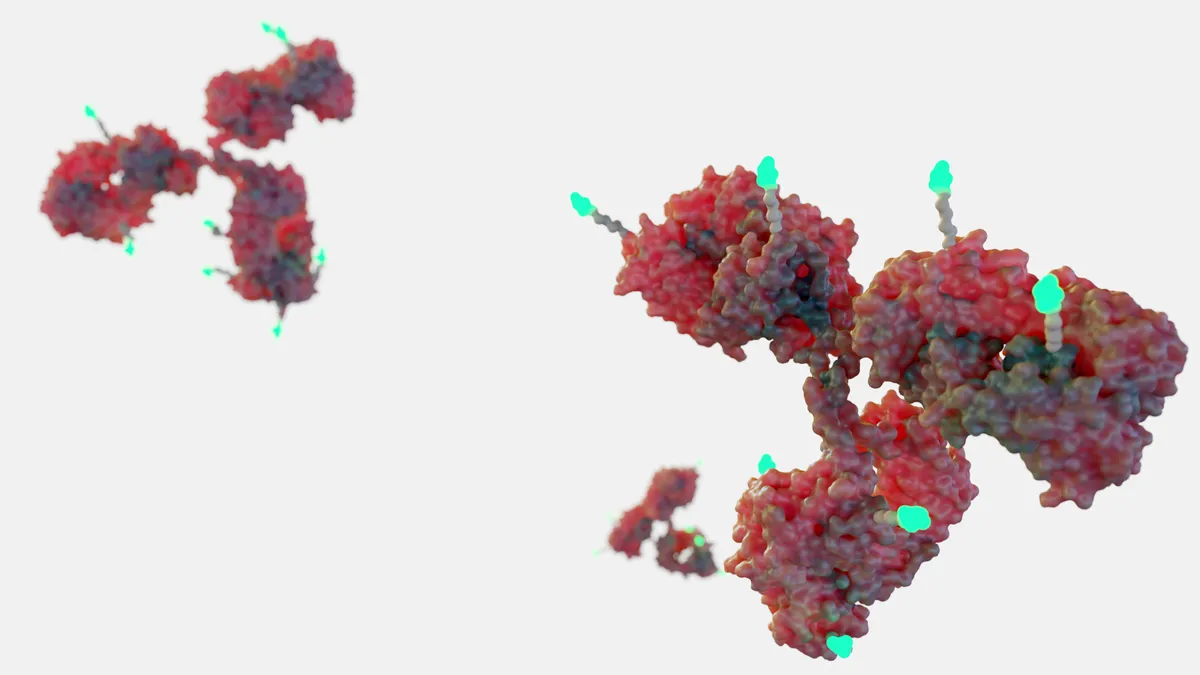
Why it matters: Wei Cao believes the company is on its way to opening up the bottleneck that has so far limited the value and efficacy of autologous CAR-T cell therapies — the laborious manufacturing process, which can take up to six weeks. While he admits Gracell is not a manufacturing company, he said it has designed a way to increase the speed of production and reduce costs. Its FasTCAR platform automates the process in a closed-loop clean suite facility to manufacture several patient samples simultaneously “using XLenti vectors derived from lentivirus,” according to the company.
“We knew if we could technically improve the manufacturing process and make it shorter, we (could not) just cut down the time, but also reduce healthcare costs linearly,” Wei Cao said. “And, by delivering the product to patients earlier we can improve outcomes, because for late-stage patients who are waiting, their disease is progressing quickly.”
The strategy: The stem cell manufacturing market is growing at a compound annual rate greater than 9% and is expected to reach more than $18 billion by 2026.
With the booming market, Gracell has plenty of competition, which Wei Cao said is “healthy,” as the goal is to make CAR-T cell therapies available for newly diagnosed cancer patients, rather than as a last-line of defense.
In late 2022, Gracell moved one step closer to realizing its goal, presenting positive phase 1 data for GC012F, which is being investigated as a first-line therapy for newly diagnosed, high-risk multiple myeloma patients. The data shows a 100% overall response rate.
“This is probably the first time there is (evidence) of safe and efficacious CAR-T therapy for newly diagnosed cancer patients,” Wei Cao said. “All these CAR-T or TCRT or any other cell and gene therapy are designed or approved for last-line therapy. So here we are, we can give this CAR-T cell therapy to newly diagnosed patients and not just to patients who run out of options.”
At a glance: The company has nine CAR-T cell therapies — autologous and allogeneic — in the pipeline, a newly established R&D center in San Diego and plans to initiate clinical trials in the U.S. in 2023.
Since 2017, Gracell has achieved several major milestones. First, it brought the conceptual design of FasTCAR to fruition.
“When that worked, it just knocked us out. A lot of people said it’s impossible you need two weeks, but we proved we can do it overnight,” Wei Cao said. “The second milestone was our IPO after three and a half years and the Nasdaq listing. The third milestone is positive data for a first-line cell gene therapy for newly diagnosed multiple myeloma or cancer patients.”
Here, Wei Cao talks more about Gracell’s newly released data around GC012F, its lead autologous CAR-T product, moving the needle to make CAR-T therapies a first-line of cancer defense, and its dual approach to increase the efficiency and reduce the costs associated with CAR-T cell therapies.
This interview has been edited for brevity and style.
PHARMAVOICE: In late December, you received positive results for GC012F. What does this mean for the program?
WILLIAM WEI CAO: This is probably the first time, forgive me if there is data outside our reach, that a CAR-T therapy has been shown to be safe and efficacious for newly diagnosed cancer patients. All other CAR-T, TCRT or other cell and gene therapies are designed or approved for last-line therapy.
“This is probably the first time there is (evidence) of safe and efficacious CAR-T therapy for newly diagnosed cancer patients."

William Wei Cao
CEO, Gracell Biotechnologies
The reason we got approved is because of our sound safety profile, 75% of our patients actually have no CRS (cytokine release syndrome). This is unheard of and beyond our expectation. CRS is a common side effect for CAR-T therapies.
We have presented data at ASH and at other conferences, so we knew the GC012F product was safe and efficacious in late-stage multiple myeloma patients. But we did not know about the data for the newly diagnosed patients for GC012F, which shows a better safety profile and 100% MRD (multiple myeloma demonstrating) negativity response. And that was a good surprise. So, we are encouraged that this signal cell therapy could be used as a front-line therapy. Because GC012F is a FasTCAR dual targeting therapy, we are investigating beyond multiple myeloma. We also have presented data for lymphoma, non-Hodgkin lymphoma and other B cell malignancies.
And then in 2023, we’ll probably announce another very big indication. FasTCAR is a sophisticated design that could enable us to use this drug in many indications.
Most companies pursue either autologous or allogeneic products. Why are you looking at both?
There are two reasons. One, we believe allogeneic is the future. Second, there (is) still a lot of research work to be done for autologous. And for these reasons we are developing both.
Autologous is a more proven technology. The first two products or three products approved in (the) U.S. and other countries are all autologous, which brings in better efficacy. Meaning, the therapeutic effect lasts longer due to the mechanism of a patient’s own cells. It tends to stay in the patient body for a longer time and has less of a chance to be rejected.
Now, off-the-shelf allogeneic CAR-T is the future. The vision is that you can manufacture many, many doses from a healthy donor. You derive the cells from a healthy donor, deploy the cells to a hospital where they can stay in the freezer and be ready to use. That sounds great. However, off-the-shelf CAR-T, which is still developing is more challenging than autologous because its other people’s cells. So genetically, these cells will not be recognized by a patient’s body as their own. There is the potential to reject the healthy donors CAR-T cells and this means the persistence or duration of these allogeneic cells in a patient’s body may not last long.