The blood-brain barrier is a cellular blockade, protecting the mind from dangerous invaders. It’s a critical safeguard but also an impediment to getting drugs into the brain that treat conditions like Alzheimer’s disease, Parkinson’s disease and cancerous tumors.
Researchers have long tried to find ways around the brain’s intricate security wall using various shuttle systems. But a new study shows the potential of focused ultrasound to boost the plaque-clearing effects of anti-amyloid-beta monoclonal antibody Alzheimer’s drugs, as well as treatments for other conditions.
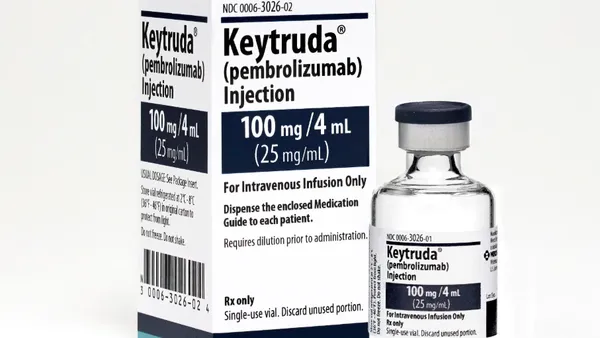
The research team used focused ultrasound alongside the recently discontinued and controversial Biogen and Eisai drug Aduhelm to treat three patients over 26 weeks. They saw a 32% reduction in toxic plaque in areas where they opened the blood-brain barrier using ultrasound.
“What we showed is that by opening the blood-brain barrier in areas that have a high density of plaques, we're able to get an accelerated reduction in beta amyloid,” said Dr. Ali Rezai, a neurosurgeon at the Rockefeller Neuroscience Institute in Morgantown, West Virginia, and the study’s lead author.
“The blood-brain barrier opening for decades has been a limitation for neuroscience therapeutics. And that limitation has now been overcome.”

Dr. Ali Rezai
Neurosurgeon, Rockefeller Neuroscience Institute
Some experts have given amyloid-clearing drugs like Leqembi a lukewarm reception because they have so far yielded relatively modest clinical improvements in patients. In a phase 3 trial, Leqembi, the first amyloid-targeting treatment granted traditional approval by the FDA, slowed disease progression in early-stage patients by 27% over 18 months — a change that might not even be noticeable to the patient, according to one expert.
“The drugs are not miracle cures, but it's the best thing we have right now,” Rezai said, noting that ultrasound technology could potentially enhance treatment efficacy, improve safety and reduce treatment time.
There’s one caveat: Even though Rezai’s study achieved faster plaque clearance in the brain, it didn’t translate into improvements for the patients measured by their ability to perform everyday tasks, although patient monitoring is still ongoing, he said. An editorial that accompanied the study noted “expanding treatment to clinically significant volumes on both sides of the brain is crucial for assessing its efficacy in slowing disease progression.”
A follow-up study, aimed at clearing plaque faster using a higher dose may result in a different outcome.
An existing technology with a new use
Focused ultrasound is already FDA-approved and reimbursed by Medicare to treat uterine fibroids and essential tremor and offer pain relief in bone cancer, among others. The technology works by directing beams of light to heat and destroy tissues in a targeted area, much like a magnifying glass can channel the sun’s rays to start a fire.
But this recent study tested a different use for the technology, pairing it with lipid microbubbles, commonly used as a contrast agent, infused through an IV. The ultrasound animates the tiny bubbles, and they expand and contract, forcing open the blood-brain barrier, Rezai said.
The treatment, guided by MRI, creates a small opening in the blood-brain barrier to deliver drugs to chosen areas of the brain. It produced few side effects, other than mild to moderate headaches in some patients, and the opening closes within 24 to 48 hours.
“It’s a brain procedure, but you're not cutting the skin or opening the skull to infuse the drug or antibody into the brain by delivering it non-invasively, which is, I think, a big leap here,” Rezai said.
In animal studies, ultrasound-assisted drug delivery achieved five to eight times the typical drug penetration in the brain, Rezai said. Currently, more than 98% of drugs do not readily cross the blood-brain barrier, which means that doctors have to use systemic treatments with high and frequent doses to achieve an effect. Opening the blood-brain barrier could allow for lower medication dosages, reducing the risk of side effects and potentially even resurrecting promising drugs shelved due to their toxicity at higher doses, Rezai said.
About the study
Rezai’s study tested the ultrasound technology in three patients with mild cognitive impairment from Alzheimer’s disease. They received ultrasound through a specialized helmet procedure alongside their monthly Aduhelm infusions for six months.
“The treatment is done in an hour and then they get off the table and they walk out,” Rezai said. The team had to move cautiously during the trial to monitor for potentially serious side effects, including brain swelling known as ARIA-E, and brain bleeding known as ARIA-H.
“It was an extremely rigorous trial. We had to have the data safety monitoring board review every step to make sure there were no safety issues before we progressed with treatment,” Rezai said.
Another trial is now in the works.
“We have FDA approval to initiate a new study,” he said. This study will not only use a different drug, Leqembi, and a higher 10-milligram dose, but the hope is to clear plaque from the brain more rapidly, in a few months rather than two years or longer, Rezai said.
Future promise
The technology is ripe for collaborations with pharma to test new applications, other than Alzheimer’s, including brain tumors, Rezai said. Pediatric brain stem cancers, which present serious surgical risks and treatment challenges are one appealing target, as are other neurodegenerative conditions such as Huntington's disease and amyotrophic lateral sclerosis (ALS).
“I think there's going to be many more centers [using the technology]. There is tremendous interest,” Rezai said.
The brain isn’t the only area of the body that could benefit — ultrasound could help deliver therapeutics to other organs by unlocking similar barriers.
But Rezai said more research needs to confirm that the technology works as intended. If it does pan out, it could one day be incorporated into the services offered at infusion centers.
“The blood-brain barrier opening for decades has been a limitation for neuroscience therapeutics,” Rezai said. “And that limitation has now been overcome.”