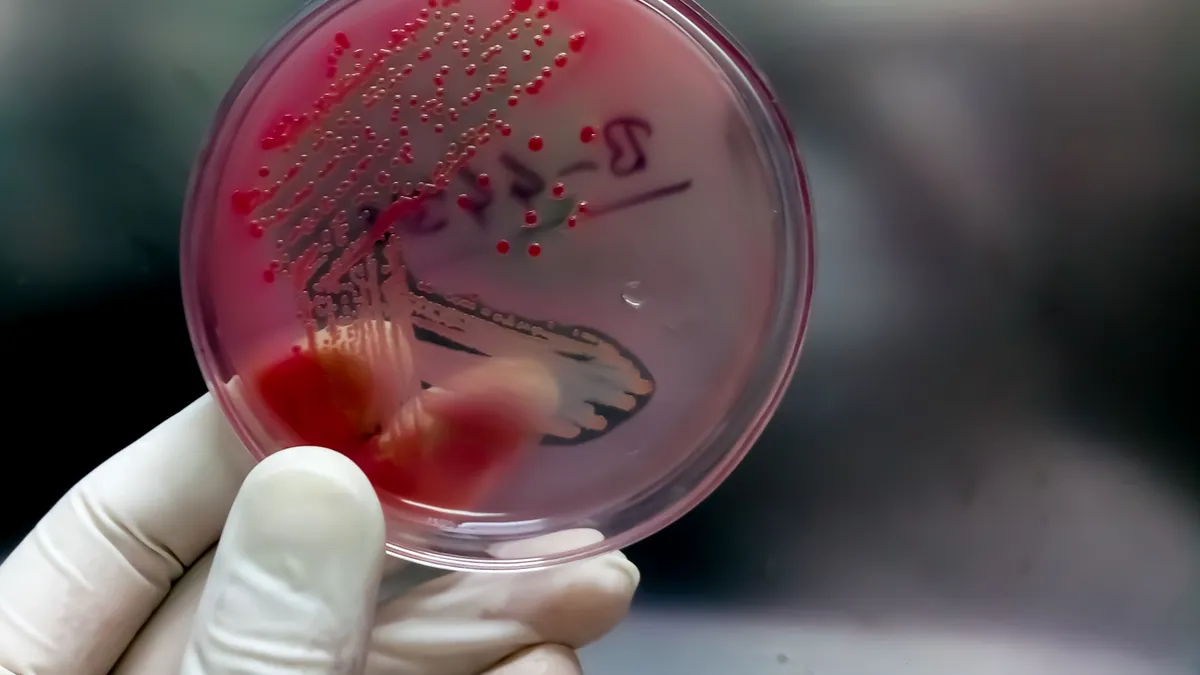
The threat of antibiotic resistance is no longer looming — it’s already here. So-called “superbug” infections killed 1.27 million people worldwide in 2019, causing more deaths than HIV or malaria. And COVID-19 has only exacerbated the problem.
Despite this gloomy outlook, attendees of the World Antimicrobial Resistance Congress held last week in Washington, D.C., appeared optimistic that a new era marked by increased government attention could be afoot.
Spurring much of that optimism was a keynote speech by U.S. HHS Secretary Xavier Becerra, who signaled that the Biden administration is strongly backing policies to incentivize the development of new antibiotics.
“Because of COVID especially, you've got the attention of the world. And more importantly, you've got the attention of Congress, you've got the attention of the most important person in the world: the president of the United States,” he said.
In March, President Joe Biden appropriated funding in his Fiscal Year 2023 budget proposal to tackle antimicrobial resistance and proposed a value-based payment model, whereby the U.S. government would pay drug manufacturers upfront to develop novel antibiotics treating the most serious bacterial threats.
The payment model aims to incentivize pharmaceutical companies who have largely abandoned antibiotic drug development over the last decade to reenter the space by providing a mechanism for them to recoup their investments.
“He's communicating to you that he gets it because it's in his budget, and as someone who has to work really hard to get HHS matters into his budget, I will tell you, he gets it,” Becerra said.
The proposal aligns with a bill introduced in Congress, dubbed the Pioneering Antimicrobial Subscriptions to End Up surging Resistance (PASTEUR) Act, which calls for increased resources to fight AMR and proposes a similar subscription-based funding model, where the government would pay drug companies a flat annual rate for novel antibiotics based on their value to public health, rather than on how many doses they sell.
Ultimately, Congress will determine whether the measure in Biden’s budget or the PASTEUR Act will become law. And it is unclear whether either will come to a vote before the current congressional session concludes in January
“The only thing we're really missing on AMR is the money,” Becerra told the AMR Congress, arguing that pharmaceutical and biotech companies have both the know-how and technology to develop new antibiotics.
“Please do not waste this moment,” he said, encouraging attendees to continue lobbying Congress for support. “Let's make this into a movement.”
‘Need it now’
Attendees of the AMR Congress saw both Becerra’s presence (he’s the first HHS secretary to attend the annual event since it began in 2015) and his message as signs of renewed progress in the mission to develop medications for antibiotic resistant infections.
“I was enormously encouraged by the Secretary of Health and Human Services really strongly supporting components of the PASTEUR Act,” said Kevin Outterson, a law professor at Boston University and the executive director of the Combating Antibiotic Resistant Bacteria Biopharmaceutical Accelerator (CARB-X), a nonprofit providing funding and support to companies developing new antibiotics.
Emily Wheeler, director of infectious disease policy at the Biotechnology Innovation Organization (BIO) trade association, also said she felt the “tide changing” at this year’s event — more so than in past years.
She noted that BIO is actively engaging members of Congress in support of the PASTEUR Act, which so far has 64 co-sponsors in the House and four in the Senate.
Lessons learned from the COVID-19 pandemic have contributed to the growing momentum. For instance, John Billington, head of commercial pipeline and health security policy at GlaxoSmithKline suggested during a keynote panel that the “warp speed” development of mRNA vaccines during the pandemic were a result of years of scientific research. Treatments for antibiotic resistance will not be created overnight, and their development must be approached in a similar manner, he said.
“The choices we make as a society to invest right now are going to be important in the future,” Billington argued, further stating that the PASTEUR Act “would be an amazing first step forward,” in bringing market certainty to antibiotic development.
Still, he, Outterson and others remained cautious about the prospect of congressional action on either the PASTEUR Act or the president’s budget.
“If we don't get it done this year, the impact will be companies that will run out of money — bankruptcies will happen and more teams will scatter and fewer drugs will eventually make it to market when we need it,” Outterson warned. “So, we need it now.”