Does Your Brand Have a Value Equation for a Changing Market?
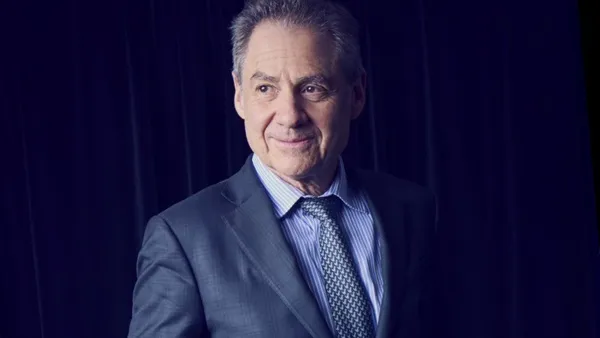
As healthcare reform gains momentum, the way pharmaceutical products are perceived by patients, providers, and payers is changing. In order to compete in the evolving healthcare marketplace, products must be positioned in a new value equation that drives positive financial and clinical outcomes. At the core of this new value equation are support services not only for patients, but also for providers and, increasingly, payers. A thorough understanding of the important role support services for different stakeholders will play across the continuum of patient care is critical to brand success. Patient Care + Improved Outcomes – the Cost of Care = Value A healthcare system predicated solely on volume of care is a thing of the past. Providing value to all stakeholders is the future. To be competitive, brands need to surround products with support services reflective of the healthcare reform mandate that puts value at the center of the system. The challenge is to provide value-oriented support to all stakeholders through innovative programs and tactics while ensuring adequate ROI. In addition to patient education and financial support programs, brands must give providers specific reimbursement support and tools for managing patient health. For payers, at what point will value-based contracts, head-to-head studies, adherence tools, and innovative patient-centered programs and resources become the new competitive advantage? For every segment — patients, providers, and payers — insightful, transparent analytics will be critical to any given program’s success. At what point will value-based contracts, head-to-head studies, adherence tools, and innovative patient-centered programs and resources become the new competitive advantage? Taregting Chronic Conditions As open enrollment in the healthcare marketplace nears, municipalities around the country are weighing their options for employees and retirees who are not Medicare-eligible. A driving force behind this is the high cost of caring for those with chronic conditions. In fact, patients with chronic conditions account for the majority of healthcare costs. According to a report by the Robert Wood Johnson Foundation, almost half of all Americans live with a chronic condition. Companies take note: the same report points out that Americans with chronic conditions use 84% of all healthcare spending, and, of those, 93% use prescription drugs. The high cost of certain treatments will continue to be a concern. The National Institutes of Health projects that spending on cancer care will increase 27% between 2010 and 2020 to $158 billion. In 2010, breast cancer ranked first in associated medical costs ($16.5 billion), followed by colorectal cancer ($14 billion). Caring for our highest-cost patients is one driver of healthcare reform. Patient-centered, coordinated, and accountable care provides a new model for efficiencies and rewards across patient populations. It is this value-based model that must be factored into a brand’s value equation. Accountable Care In keeping with the reform-mandated emphasis on value, accountable care organizations (ACOs) are placing greater weight than traditional care models on drug outcomes, overarching quality measures, and patient satisfaction. Although their success has been hotly debated in the national media, all 32 Pioneer ACOs earned incentive payments in their first year for their quality measure reporting, according to the Centers for Medicare and Medicaid Services. To compete with generics within the ACO structure, brand name drugs are going to have to spend more on patient support programs that measurably improve patient outcomes. When providing value is the primary goal, it will no longer be enough to claim better outcomes over generics. Which takes us back to the idea of value-oriented support. All programs — for patients, providers, or payers — will have to show in quantifiable terms how they are delivering value by improving patient outcomes. For patients, brands will need to provide programs on, for example, how diet and exercise can impact health. Brands will then need to successfully market the improved outcomes garnered from these patient programs to providers and, increasingly, to payers. Analytics will be used to address every patient population in the payer segment, from the new customers signing up for healthcare for the first time, to existing Medicare patients. Innovative analytics will be used to forecast every aspect of the new healthcare system, from allocating provider resources to anticipating individual patient needs. The Future of Value To survive in the new age of healthcare, pharmaceutical brands must continue to adapt to change. Instead of a product-centered focus on better formulary placement or fewer restrictions, marketers must consider value. Product launches will be targeted to smaller, better-defined audiences. Brands must be included in — or at least follow — national guidelines, the sooner after launch the better. Disease education, data collection, and patient follow-through must be spelled out. The impact of this focus on value will organically lead to a familiar goal: a robust bottom line. Today, marketers need to embrace the shifting market by surrounding a product with a compelling suite of strategies and programs that will build payer belief in a brand. Dan Sontupe Executive VP, Payer Strategy and Market Access The CementBloc At what point will value-based contracts, head-to-head studies, adherence tools, and innovative patient-centered programs and resources become the new competitive advantage? The CementBloc is a multichannel healthwellness communications company based in New York City. Founded in 2000 by Susan Miller Viray and Rico Viray, The CementBloc is also a founding member of Indigenus, an independent global network of entrepreneurial healthcare creative agencies. { For more information, visit thecementbloc.com. { For more information on how to maximize your brand’s effect on the value equation, contact Dan Sontupe at The CementBloc: [email protected].