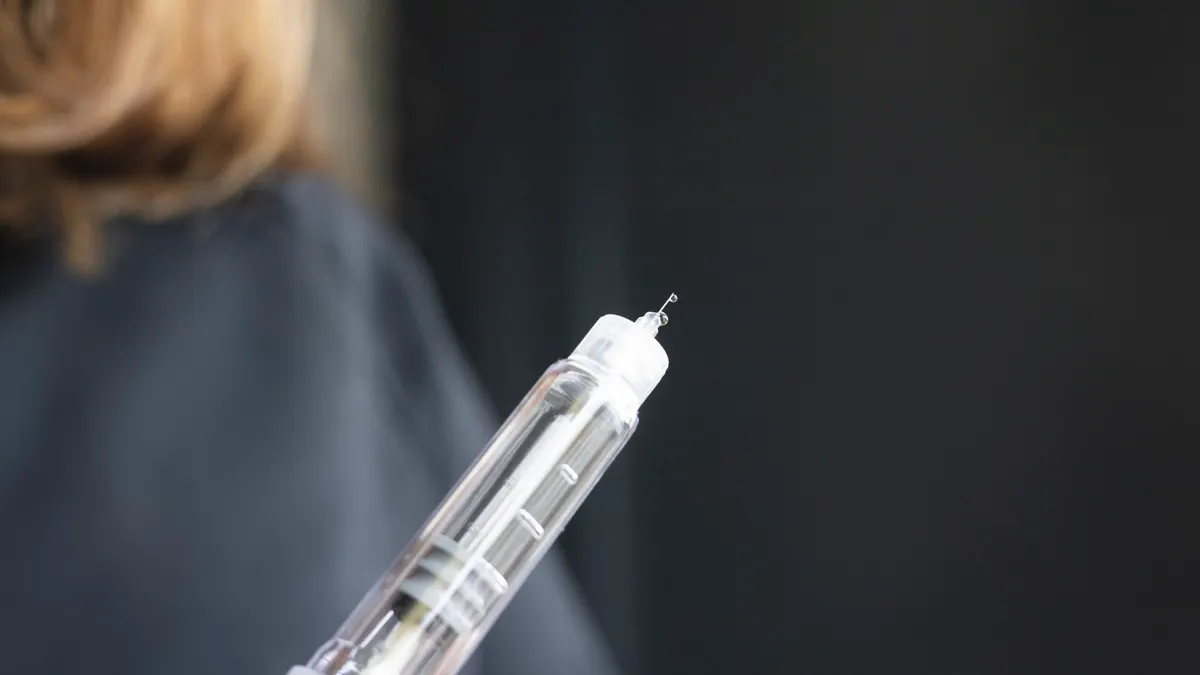
Despite the decades of R&D and billions spent to bring game-changing drugs like GLP-1s to market, efforts to make sure patients inject the drugs properly have come up short.

While prescriptions for updated diabetes medications have skyrocketed, education about injection techniques have fallen by the wayside, said Pasha Javadi, senior director of medical affairs at Embecta, a Becton Dickinson spinoff that specializes in syringes and pen needles for people with diabetes.
“Insulin, and recently GLP-1s, are treating millions of people with diabetes, and usually many people don’t get the full benefit of those,” Javadi said. “The key subject most healthcare practitioners talk about is the drug and the treatment side — the injection part of administering the drug to the body is most of the time overlooked or considered a given.”
Javadi and a group of diabetes specialists from around the world recently updated the best practices for insulin and noninsulin injection techniques originally published in 2016 for a more comprehensive and accessible standard across diabetes medications.
And for drugmakers relying on clinical and real-world results bolstering prescriptions and sales of their products, standardized procedures and education for injections could not only make a difference for their patients but also for the future of their medicines.
“By changing the practice even a little bit, you can significantly increase [blood glucose] reduction, which comes at zero cost,” Javadi said. “And since 2016, there [have been] so many different changes not only on the technology side, but from the drug perspective.”
In today’s world of shifting diabetes practices, structured training for healthcare professionals and education for patients are both critical to getting the most out of standbys like insulin and newer options like GLP-1s.
Adapting to the new norm
Updates made by the Forum for Injection Technique and Therapy Expert Recommendations, or FITTER, were based on new tech and drugs, but were also created to improve communication to healthcare professionals as they convey cutting-edge diabetes treatment procedures to their patients.
“One of the key questions out there for GLP-1s is that people receiving it have never had any education on the injection techniques,” Javadi said. “And not all needles and not all syringes are equal in a way that impacts people’s injection experience and also their glycemic control.”
While adapting to new treatments presents challenges on the education front, it’s still a good position to be in, Javadi said.
“Newer drugs are an opportunity for new and better choices for the patient,” Javadi said. “When GLP-1s came to the market, it’s an added tool for a person with diabetes, and there’s no concern there — where there is concern is the education gap in how to use them.”
As millions receive the latest blockbuster drugs from Eli Lilly or Novo Nordisk — and in some cases clamor for them — the new set of patients need to learn how needles work, which isn’t always intuitive.
“The key subject most healthcare practitioners talk about is the drug and the treatment side — the injection part of administering the drug to the body is most of the time overlooked or considered a given.”

Pasha Javadi
Senior director of medical affairs, Embecta
Patients who don’t know how to inject a GLP-1 or receive the product without pen needles because they weren’t aware they come separately often report their struggles to Embecta. Some might inject the drug into muscle instead of fat, where it’s intended.

“Not enough time is given to help someone understand how to get the most out of the pharmaceutical product they’re being prescribed,” said Ginny Blocki, senior vice president of strategy at Embecta. “What the scientific community gathered to talk about was how to ensure that someone doesn’t get a prescription, get home and then say, ‘Now what?’”
Even a short tutorial from a nurse or healthcare educator can make a big difference, Blocki said.
From a drugmaker’s perspective, a structured injection education program helps take the “whole patient experience” into account and ensure the most benefit from the drug, Blocki said.
Staying up to date
Insulin is “still the key solution for people with diabetes” despite GLP-1s elbowing into the space, especially in Type 1.
“For Type 1 diabetes, there is only one thing, and it’s insulin,” Javadi said. “If you put aside the buzz of the media in clinics, Type 1 has no other choice.”
For Embecta, that means having a foot in both worlds — keeping the older insulin products flowing for those who need them while staying up to date with newer medications like GLP-1s.
“We’ve been around for over 100 years, and we’re very proud of the fact that we keep up to date on anything about delivery, from a pen injector to a vial and syringe,” Blocki said.
It’s critical that pharma companies and medtech developers adapt together rather than separately.
“It’s on us as much as it is on the pharmaceutical companies to ensure there is a partnership in helping people understand how to get a better experience of delivering their drug,” Blocki said.
Not every product fits into existing market priorities — despite receiving FDA clearance for an insulin patch pump last year, for instance, Embecta chose not to continue with the program, cutting 125 jobs from the workforce.
“The reality is, although there will be newer products, we will always have pen needles or vials and syringes,” Blocki said. “We want to make sure we have something that might help patients with a better injection experience.”
And connecting patients’ individual needs with a drugmaker’s latest product is a devicemaker’s sweet spot.
“It’s more than just getting a prescription,” Blocki said. “How do you satisfy [a patient’s need] from the very beginning to the very end with a complete knowledge of what has to be done and how to do it? That can be different for every patient.”