Welcome to the Biotech Spotlight, a series featuring companies creating breakthrough technologies and products. Today, we’re looking at Tessera Therapeutics, a preclinical biotech from Flagship Pioneering developing a new class of genetic medicines.
In focus with: Michael Severino, CEO, Tessera Therapeutics
Severino’s vision: As the former president and chief scientific officer of AbbVie, Severino is one of many Big Pharma execs who’ve jumped aboard a Flagship Pioneering-affiliated company in the past year. He took the helm of genetics-focused Tessera in June 2022 and said the switch felt like a “homecoming.”
“When I was thinking about what made sense for the next chapter, it was about opportunities — where I could do cutting-edge basic science that can be applied to patient care and develop important new drugs,” he said.
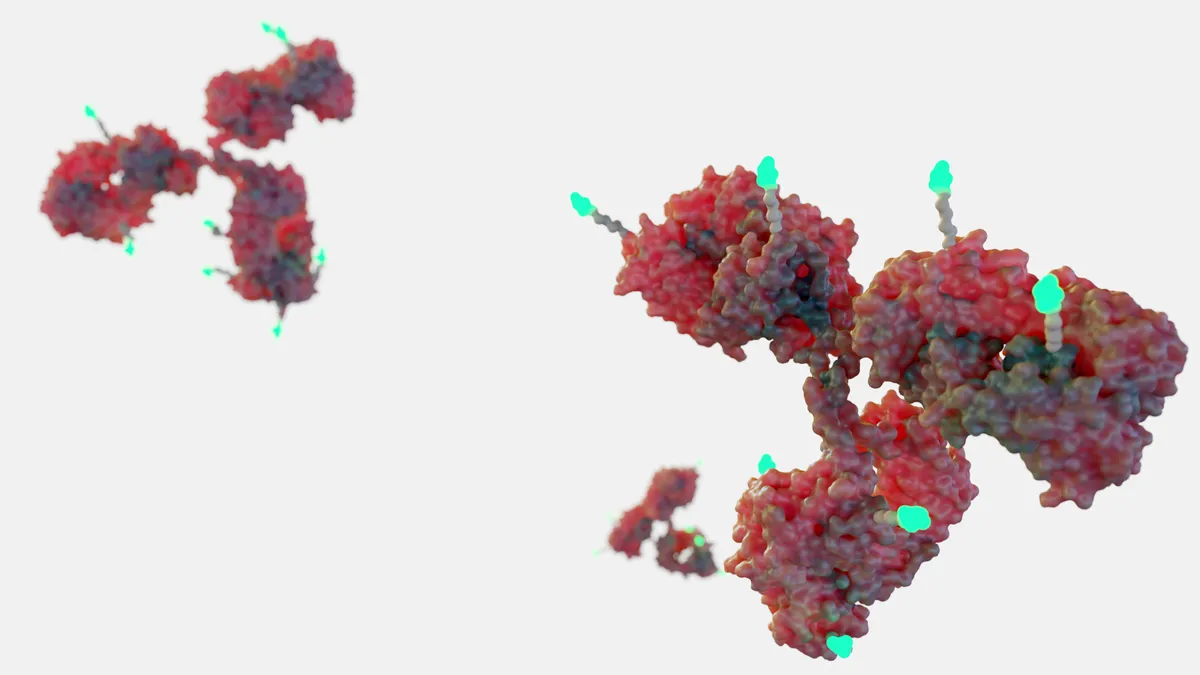
At the preclinical biotech Tessera, he’s aiming to develop a new class of genetic medicines that harness mobile genetic elements — pieces of genetic material that transport DNA and code for enzymes and proteins — to potentially “make any type of genomic alteration needed to treat or cure disease.”
At a glance: Tessera’s gene writing platform includes three systems — DNA gene writers, RNA gene writers and RNA gene rewriters — that can swap base pairs, insert DNA sequences or rewrite portions of the genome, all within the body.
The company is testing the technology in mice and nonhuman primates for liver, blood and immunology indications. This spring, it presented primate data for treatment of the rare inherited condition phenylketonuria caused by a genetic mutation. After one injection, the drug altered base pairs in up to 45% of animal cells, far surpassing the 10% curative threshold required.
Additionally, in a sickle disease study, the technology reversed the mutation that misshapes red blood cells to.
Why it matters: Unlike other genetic platforms like CRISPR-Cas9, Tessera’s technology could one day rewrite genes in the body, eliminating potential manufacturing hurdles and bottlenecks, Severino said. If it is shown to be effective in humans, Tessera’s MGE approach would let scientists swap or edit any base pairs, opening the door for treatment of many genetic diseases.
“Nobody has the technology to truly correct that mutation of wild type …outside the body without a stem cell transplant to readminister,” Severino said. “If we can put all those pieces together, we can have a game-changing opportunity not only for our company, but for patients.”
Here, Severino discusses his decision to join Tessera, his vision for curing any genetic disease with the company’s technology and how he’s charting a path to get there.
This interview has been edited for brevity and style.
PHARMAVOICE: You're one of many Big Pharma execs to have joined Flagship in the past year. What's in the water at Flagship? What is it about the company that made you want to join?
MICHAEL SEVERINO: I think it's the level of innovation that goes on around the Flagship ecosystem. Flagship doesn't think of itself as a traditional venture capital company — it doesn't invest in other people's ideas. It looks for ways to create completely novel platforms that have the potential to produce important new drugs or meet other needs in either biomedical sciences or other related areas, and that focus on innovation really resonates with me. I think that's the attraction for many of my peers who've joined Flagship as well. They have that focus and the commitment to see it through and the experience from having done it before. It's hard to find all those features in one place. And when you do, it's something special.
You said earlier this year that Tessera aims to “cure nearly any genetic disease, reduce the risk of common disease and do this broadly and efficiently across patient populations.” Why are you confident that you’ll reach these lofty goals?
That potential exists because we're developing the toolkit that's necessary to make whatever changes are needed in the human genome to address disease. We don't just have a single technology. We don't have just one approach for a certain kind of genetic alteration. If we need to change one letter in the human genome, we have the technology to do that. If we need to write longer segments into the human genome, we have the technology to do that. And so that gives us tremendous power. We leverage that power even further by developing the delivery mechanisms that are necessary to do it in living systems and, ultimately, in patients. It doesn't really matter if you have the best gene editing machinery in the world. If you can't get it where it needs to be in a patient, you can't make that kind of impact.
What about the preclinical trials you’ve conducted gives you confidence in this technology so early?
We've done work that gives us proof of concept in a number of preclinical models of disease, in mouse models and in nonhuman primates. In genetic medicine, those give a high degree of confidence for success in the clinic, and the reason is that we know unambiguously what the cause of the disease is. If we're treating a genetic disease like phenylketonuria or alpha-1 antitrypsin (AAT) deficiency, or sickle cell disease, we're not trying to use that animal model to figure out what the cause of the disease is. We're using the animal model to determine: Can we deliver in a living system and does the gene writing machinery work in the same way in a nonhuman primate, for example, as it did in all our work in cell lines and in human cells in vitro? When the answers to those questions are yes, history tells us that it has a high probability of translating into the clinic.
As a leader, how do you lay out baby steps toward that broader goal?
We're going to prioritize diseases that are the clearest fit for our technology today and look at how it can grow and evolve in the future. So, the clearest fit for the technology today might be tissues that we can deliver to —we can deliver to the liver, to bone marrow stem cells, to immune cells in particular T cells that might be relevant for cancer applications.
There are many other monogenic diseases caused by a single mutation in the genome that can fit that pattern that we’ll go after. We can look at how we might be able to reprogram immune cells in vivo so that we don't have to have a monthlong manufacturing and waiting process and the need to give chemotherapy as conditioning before we administer cell-based therapy and think about how that can be applied to cancers.
As we demonstrate value, we can also take on more biological risk. We can take on common diseases where there may not be one single cause, but we have a good idea of changes that we can make in the genome to reduce the risk of disease or to even prevent disease. So we start with the base of what we know we can do today and then continue to expand out almost in concentric circles.
What does that look like in the next year and beyond?
We want to keep developing that platform. Our platform is outstanding, but no platform is ever good enough. We want to gain more information in preclinical models, do more work in large animal models and in nonhuman primates to set ourselves up for the clinic and in the not-too-distant future, a clinical company with proof of concept in patients for our technology. Now, obviously, the goal is to get these therapies approved and help patients in clinical practice.